We Answer Your Latest Questions about Remote Therapeutic Monitoring: From How It Works to How to Bill

Note that this article is the first part of a series. You can read part two here.
The new remote therapeutic monitoring (RTM) CPT codes have opened up new possibilities for many providers, along with a number of questions about how RTM works and how to bill for it. To help you navigate the new billing codes and workstreams, here are answers to some of the questions we most commonly receive related to RTM.
What is remote therapeutic monitoring (RTM)?
Remote therapeutic monitoring (RTM) services monitor non-physiological health conditions, including the status of the musculoskeletal system, respiratory system, and therapy adherence.
Over the last year, a new set of billing codes has been implemented and is in the process of being refined by the Centers for Medicare and Medicaid Services (CMS). This set of codes allows clinicians to be reimbursed for tracking and reviewing patient information using medical devices (including certain software) that can perform remote monitoring.
Why is RTM important?
Providing remote care to patients via high-quality digital healthcare technologies improves access to care, resulting in better patient outcomes, satisfaction, and retention. And with the new codes, providers can now be reimbursed for providing that additional care to Medicare patients, which was not previously possible.
We expect that as medical device technology continues to improve in tandem with our ability to make use of the resulting data, the trend toward monitoring patient status remotely will continue. And the new codes indicate that CMS also recognizes and is invested in the importance of digital care for rehab.
Who can bill for RTM?
RTM is available to all qualified health care practitioners who are not eligible to independently bill for evaluation and management. This includes PTs, PTAs, OTs, COTAs, and more.
What are the new RTM codes and how are they billed?
There are five new CPT codes for RTM. This list includes what they are, what they cover, and how they’re used.
CPT Code 98975: Device Education and Onboarding
What’s Covered
Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response), initial set-up, and patient education on use of equipment.
Clinical Example
If you talk with your patient about a home program, help them log into the app, and provide an overview of how to navigate the app, you’ve met the set-up and education requirements for this code. Once monitoring has occurred for 16 days in a 30-day period, you can be reimbursed for that time.
How It’s Used
- Report this code once per episode of care.
- Only report if monitoring occurs over at least 16 days.
More Information
Billing for CPT Code 98975
CPT Codes 98976 and 98977 (Device Supply)
What’s Covered
Remote therapeutic monitoring (e.g., respiratory system status, musculoskeletal system status, therapy adherence, therapy response), device(s) supplied with scheduled (e.g., daily) recording(s) and/or programmed alert(s) transmission, each 30 days.
Code 98977 refers to monitoring of the musculoskeletal system, and 98976 refers to monitoring of the respiratory system.
Clinical Example
When your patient accesses their program from home, each day they complete exercise activity, respond to surveys, or send messages counts towards the 16 scheduled recordings. Once they’ve logged 16 such days within a 30-day period, you can be reimbursed via this code.
How It’s Used:
- Make sure to use the appropriate code based on the system being monitored.
- Only report these codes if the patient has had at least 16 scheduled recordings and/or programmed alerts transmitted in a 30-day period.
More Information
Billing for CPT Code 98976 and 98977
CPT Codes 98980 and 98981 (Remote Treatment)
What’s Covered
Remote therapeutic monitoring treatment management services, physician/other qualified health care professional time in a calendar month requiring at least one interactive communication with the patient/caregiver during the calendar month.
Code 98980 refers to the first 20 minutes of provider time during the calendar month, and 98981 refers to each subsequent 20 minutes of provider time during the calendar month.
Clinical Example
When you spend time calling your patient, reviewing patient activity, responding to messages, and updating your patient’s program, it all counts towards 98980 and 98981. Log your time as you go, and at the end of the month, if you’ve spent at least 20 minutes completing these activities and had one interactive communication, you can be reimbursed for that time via this code.
How It’s Used
- Code 98980 should only be billed once each calendar month. Code 98981 can be billed multiple times for each additional 20 minutes of activity after the first 20 minutes.
- One interactive communication needs to occur for each calendar month in which you bill these codes. For example, if you record 40 minutes of activity within a calendar month, you can bill for both codes as long as at least one interactive communication session has occurred.
- Provider time includes time spent reviewing patient activity, responding to messages, updating HEP programs, and communicating with patients interactively.
- Refer to your organization’s guidelines to ensure you know what activity to log and submit for reimbursement.
More Information
Billing for CPT Code 98980 and 98981
For more detailed information about each CPT code, please refer to the article What are the new RTM CPT codes?
How do I know when 16 days of activity have been completed by my patient?
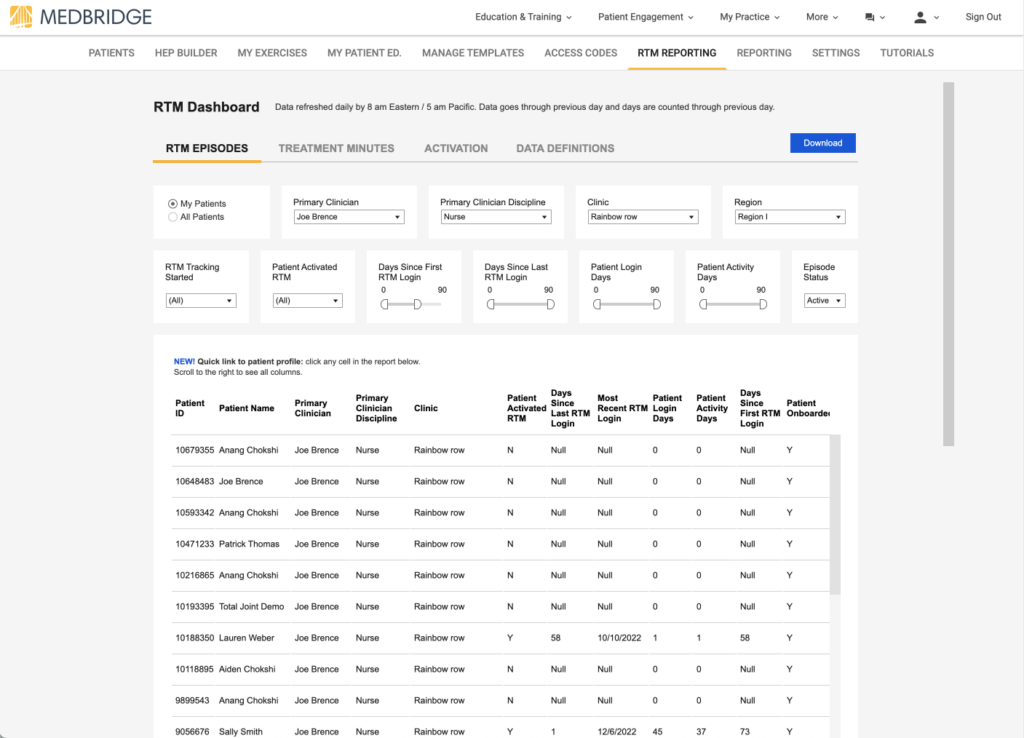
If you’re using MedBridge, you can use the RTM Reporting page (see image below) to review activity for all your patients. Organizations have varying interpretations of what a day of monitoring entails as it relates to these CPT codes.
With MedBridge, you’ll use one of the following three filters (depending on your organization’s policy) to determine activity data:
- Days Since First RTM Login: The total number of days since the patient first logged in (i.e., activated) after RTM was enabled for the episode of care.
- Patient Login Days: The total number of days where a patient login occurred after RTM was enabled for the episode. If a patient logs in multiple times on a single day, that day will only be counted one time.
- Patient Activity Days: The total number of days that the patient completed an activity, as defined below, after RTM was enabled for the episode. If a patient completes multiple activities on a single day, that day will only be counted as one day.
Patient activities—logging adherence, engaging with education resources, messaging their clinician, reading a message, viewing an exercise or education video, completing a survey
Your organization should determine which approach is right for your organization’s needs. Always refer to your organization’s guidelines when submitting for reimbursement.
The MedBridge RTM Reporting Page
How is interactive communication defined?
As it pertains to the RTM CPT codes, interactive communication is defined as remote communication that includes two-way audio communication. This usually means a phone call or telehealth virtual visit. You can log any interactive communication that occurs from the RTM Activity Log on the patient’s profile, making it easy to know when you’ve met this threshold.
What payers will reimburse for RTM billing codes?
At this time, only Medicare has confirmed they will reimburse for RTM billing codes. However, there has been some indication that other payers may reimburse for RTM in some regional areas and/or in the future. Work with your organization to determine if any additional payers are reimbursing for RTM.
Are the RTM codes subject to multiple procedure payment reduction (MPPR)?
No. CMS designated the RTM codes as “sometimes therapy” codes, which means that while they will count toward the annual therapy threshold, MPPR will not apply.
Are the RTM codes subject to the PTA/COTA payment differential?
RTM codes 98975, 98980, and 98981 will be subject to the payment differential (15 percent reduction) if provided in whole or in part by a PTA/COTA. RTM codes 98976 and 98977 will not be subject to the payment differential (i.e., the de minimis standard).
If my patient starts toward the end of the month, and I’m not able to record 16 days of monitoring within the same month to bill for 98976/98977, can I still bill for 98980/98981?
Yes, you should be able to bill for 98980/98981 if you meet the time requirement of 20 minutes or more and conduct at least one interactive communication.
Does 98975 require 98977 to be fulfilled to be billed?
Based on our interpretation of the guidance provided by CMS and AMA, 98975 is independent of 98977. The two codes can be considered and billed for individually, and 98977 does not need to be fulfilled in order for you to bill 98975.
Furthermore, in 2022, it was proposed that these codes be revised to explicitly state that these two codes are dependent on each other, but ultimately CMS did not include that update in their 2023 final rule.
Code 98975 refers to the provider setting up the device, educating, and setting expectations for use of the device with the patient and/or caregivers. Once the patient logs in and sets up their device, they have the ability to use the device, so the code starts to become eligible. Sixteen days after that patient first logs in, you can bill for 98975.
Code 98977 requires schedules or programmed alerts to be transmitted on 16 out of 30 days. Therefore, the patient needs to log in to MedBridge and complete some activity in order for a day to be counted toward the 16-day threshold. So while you can bill for 98975 if the patient has access to their device for 16 days, you cannot bill for 98977 until the patient has provided data on 16 days.
As always, defer to your organization’s guidelines as their interpretation of the CMS code may differ.
How can MedBridge help with RTM?
The MedBridge Remote Therapeutic Monitoring Solution includes our Home Exercise Program (HEP) Builder, Patient Mobile App, and Patient Portal, and meets the FDA’s definition of a Medical Device that is eligible for billing against CMS’s new RTM codes.
To help our clinicians bill against these codes, MedBridge has built a comprehensive digital platform that allows providers to onboard patients and assign them a digital home exercise program (HEP) that includes education and exercises. Once HEP programs are assigned, providers can track patient engagement with the HEP, update and modify programs for remote treatment, and facilitate communication between the patient and their care team, all from within the MedBridge RTM solution.
Our solution allows clinicians to track patient device onboarding and the time spent reviewing the resulting data. MedBridge also provides patient data monitoring and maintains all of the required auditable documentation.
Does MedBridge meet the FDA requirements for a medical device as described in the new CPT codes?
Short answer: Yes!
Just like the patient monitoring codes (a separate set of CPT codes), the RTM codes require that any device used for monitoring must meet the FDA’s definition of a medical device (as opposed to, for example, a general wellness device). The MedBridge GO App and MedBridge Patient Portal were reviewed by an independent party and determined to meet the FDA’s definition of software as a medical device.