The Pain and Disability Drivers Model: Personalizing Care for Patients with Musculoskeletal Conditions

Become an expert in orthopedics with MedBridge’s Orthopedic Excellence Certificate series. Gain evidence-based insights into assessment and treatment for the spine, upper quarter, and lower quarter to relieve patient pain and improve their quality of life.
Let’s speak frankly.
Despite an investment of millions of dollars and thousands of studies examining best treatment approaches, we’ve plateaued in our efforts of improving patient outcomes.1 In fact, we have not just plateaued, we’ve declined.
Why Are Outcomes Worsening?
As with all things associated with healthcare, the reasons for our decline are multifactorial. It is well documented that clinicians often fail to heed guideline-oriented care,2 providing predominantly low-value options that frequently fall short of improving the patient’s condition. It is also well documented that patients’ concomitant disorders have contributed to their overall health status and have caused lower outcomes in region-specific conditions such as low back pain, shoulder pain, and neck pain.3 Simply stated, today’s generations of patients are less healthy than comparative previous generations.4
A lesser-known fact is that most of the treatment options of musculoskeletal disorders have small specific effects, rendering the likelihood of large improvements associated with the treatment unlikely. Specific effects are those that are unique to the application of the treatment. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) have specific analgesic effects and long-term anti-inflammatory specific effects when used consistently. These specific effects can contribute (in a small way) toward the overall recovery of someone suffering from nociceptive pain and inflammation.
Unfortunately, for the majority of individuals with musculoskeletal disorders, there is no silver bullet treatment option that has a strong specific effect.
In fact, the majority of change we see in most patients over time is associated with natural history and non-specific effects. Natural history is the usual course of development of a disease or condition, especially in the absence of treatment, and for most musculoskeletal disorders, the natural history is favorable.
Non-specific effects are those unrelated to natural history and specific effects, and they are influenced by placebo, patient preferences, therapeutic relationships, or shared mechanisms. This is illustrated in Figure 1, which gives some perspective on the overall contributors to recovery and why any intervention tends to be more successful than no intervention.
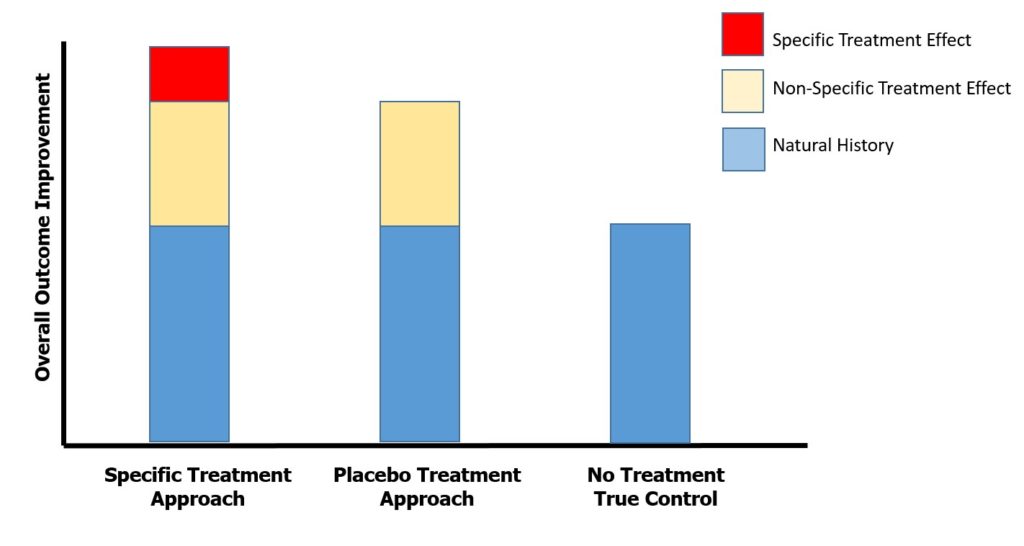
Figure 1. The theoretical contributions of specific effects, non-specific effects, and natural history in the recovery process of a patient with musculoskeletal disorders
With such small projected specific effects, it’s easy to see why the wrong care often leads to a lack of comparative notable improvement for studies involving patients suffering from musculoskeletal disorders. It also suggests that providing the right care—care that is explicit to the patient—could be helpful in improving patient-reported outcomes. This approach may reduce the challenges associated with small effects. An approach that targets each contributor to the pain and disability of a patient may have an “additive effect,” thus compiling the small effects toward a much larger effect.
Personalized Care Options: Missing in Action
To me, the most compelling reason why we have seen a decline in outcomes associated with musculoskeletal-oriented care is a lack of personalized care options, often described as the right care for the right patient.
Personalized care—or precision medicine—involves tailoring medical treatment to the individual characteristics and presentations of each patient. Personalized medicine is built on the assumption that there are highly variable responses to pharmacological5 and non-pharmacological6 treatments among care recipients, even when using evidence-based treatment approaches.
Providing personalized care requires an understanding of all the potential drivers behind the pain or disability that each patient experiences.
An underlying assumption of personalized care is that a “one size fits all” approach to care does not work. Even a classic biomedical-oriented diagnosis such as patellofemoral pain syndrome may actually exhibit multiple phenotypes.7 Phenotyping relies on an understanding of how a person’s unique clinical presentation, behaviors, and genetic profile make them susceptible to disabilities.8 Subgrouping patient-types that include psychological, social, and biological elements may further personalized care options unique to the patient being examined.
The Pain and Disability Drivers Model
The Pain and Disability Drivers Model (PDDM) was created to identify the primary drivers of pain and disability, which are unique to each patient.9
As seen on Figure 2, the PDDM involves standardized assessment elements within five domains of pain and disability:
- Nociceptive drivers
- Nervous system dysfunction drivers
- Comorbidity drivers
- Cognitive-affective drivers
- Contextual drivers

Figure 2. The Pain and Disability Drivers Model
The PDDM has been implemented in selected Canadian health systems and has been effective in prioritizing care choices for clinicians for all forms of musculoskeletal injuries. The tool is easily implemented into clinical practice, as it requires dedicated queries during the assessment for each of the five specific domains. Content validity has been assessed, and a recent Delphi study helped define the specific queries that are appropriate for each domain.10
The PDDM is used to improve the specificity of the personalized care options (problems specific to each patient). This is unique, since most classification systems and guidelines reflect only nociceptive pain drivers.
What Is the Next Step in Implementing the PDDM into Practice?
The PDDM is an open source tool available for all individuals.10 The tool promotes a biopsychosocial approach to the care of each patient, making it important to understand this process conceptually when working with patients.11
Personalized medicine has been called an “audacious aspiration.”12 We feel the PDDM is an audacious step in the right direction for care of patients with musculoskeletal disorders.
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. (2016). Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet, 388(10053),1545–1602.
- Zadro, J., O'Keeffe, M., & Maher, C. (2019). Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ Open, 9(10), e032329.
- Rundell, S. D., Patel, K. V., Krook, M. A., Heagerty, P. J., Suri, P., Friedly, J. L., & Turner, J. A., et al. (2012). Multi-site pain is associated with long-term patient-reported outcomes in older adults with persistent back pain. Pain Medicine, 20(10),1898–1906.
- Blue Cross Blue Shield. (2019). The Health of Millennials [Report]. Retrieved from https://www.bcbs.com/the-health-of-america/reports/the-health-of-millennials
- Vogenberg, F. R., Isaacson Barash, C., & Pursel, M. (2010). Personalized medicine: part 1: Evolution and development into theranostics. Pharmacy & Therapeutics, 35(10), 560–576.
- Edwards, R. R., Dworkin, R. H., Turk, D. C., Angst, M. S., Dionne, R., Freeman, R., & Hansson, P., et al. (2016). Patient phenotyping in clinical trials of chronic pain treatments: IMMPACT recommendations. Pain, 157(9), 1851–71.
- Selfe, J., Janssen, J., Callaghan, M., Witvrouw, E., Sutton, C., Richards, J., & Stokes, M., et al. (2016). Are there three main subgroups within the patellofemoral pain population? A detailed characterisation study of 127 patients to help develop targeted intervention (TIPPs). British Journal of Sports Medicine, 50(14), 873–880.
- Diatchenko, L., Fillingim, R. B., Smith, S. B., & Maixner, W. (2013). The phenotypic and genetic signatures of common musculoskeletal pain conditions. Nature Reviews. Rheumatology, 9(6), 340–350.
- Tousignant-Laflamme, Y., Martel, M. O., Joshi, A. B., & Cook, C. E. (2017). Rehabilitation management of low back pain—it's time to pull it all together! Journal of Pain Research, 10, 2373–2385.
- Tousignant-Laflamme, Y., Cook, C. E., Mathieu, A., Naye, F., Wellens, F., Wideman, T., Martel, M.-O., & Lam, O. T.-T. (2020). Journal of Evaluation in Clinical Practice, 26(1), 316–325.
- Kusnanto, H., Agustian, D., & Hilmanto, D. (2018). Biopsychosocial model of illnesses in primary care: A hermeneutic literature review. Journal of Family Medicine and Primary Care, 7(3), 497–500.
- Dzau, J. D., Ginsburg, G. S., Chopra, A., Goldman, D., Green, E. D., Leonard, D. G. B., & McClellan, M., et al. (2016). Realizing the full potential of precision medicine in health and health care: a vital direction for health and health care. NAM Perspectives. Retrieved from https://nam.edu/realizing-the-full-potential-of-precision-medicine-in-health-and-health-care-a-vital-direction-for-health-and-health-care/