Dysphagia Assessment: Have You Considered the Esophagus?
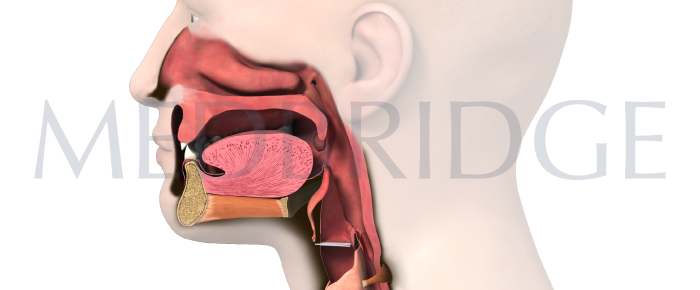
To perform accurate diagnostic assessment, we must understand the interrelationship between all stages of swallowing. Even though the speech-language pathologist does not diagnose esophageal-based disorders, we need to know when to refer to a gastroenterologist for further diagnostic testing. Without this knowledge, the patient may be denied appropriate services that explain the reason for their dysphagic complaint.
The cause may not be where you’re looking
It is too easy to miss an esophageal disorder when the patient’s complaint is focused in the oral and pharyngeal regions. Patients may localize their complaints to the neck when the primary disorder is in the esophagus. Patients with distal narrowing of the esophagus, for example, often point to the pharyngeal region to indicate where they sense an obstruction. Patients with esophageal achalasia often refer their symptoms to the neck.
We must always remember that the stages of swallowing (oral, pharyngeal, and esophageal) are interdependent. What happens upstream can affect succeeding events downstream. Even more pertinent to primary esophageal disorders is their potential impact on what is happening upstream in the oral and pharyngeal stages of swallowing.
Obstructed Esophagus
Consider how an obstructed esophagus might affect subsequent oral and pharyngeal swallows. When a series of boluses fail to clear the esophagus, attempts to pass additional boluses from the pharynx into the esophagus may be unsuccessful. In this example, it is possible that the oral or pharyngeal stage may appear to be abnormal, and that the primary problem rests there. However, if clinicians fail to image the esophagus, they may miss the primary source of the oral or pharyngeal abnormality. Similarly, if the patient’s dysphagic complaints are localized to the neck and the oral and pharyngeal stages are normal, there is a need to image the esophageal stage as a possible explanation for their complaint.
Scleroderma
Even in cases with less dramatic esophageal pathology, whether structural or motor in nature, there can be a variety of anomalies apparent in oral and pharyngeal function. Scleroderma, a disease that destroys connective tissue throughout the body and impairs esophageal peristalsis, often has secondary effects on pharyngeal function. With the pharynx being impacted by the likelihood of proximal reflux, these patients often complain that they have to expend an inordinate amount of energy to initiate pharyngeal swallows to compensate for inefficient esophageal peristalsis.
Speech-language pathologists specializing in dysphagia must have a working knowledge of esophageal disorders and understand how various stages of swallowing interact. Patients rely on our thorough, accurate assessments and, when necessary, timely referrals. To perform an accurate diagnostic assessment, a clinician must not only visualize the esophageal phase of swallowing, but also must take a careful history using the decision tree described at the end of this presentation.









