Four Factors of Patellofemoral Pain Syndrome
In a previous post, we discussed the utility of Vastus Medialis Obliquus strengthening in the treatment of Patellofemoral Pain Syndrome (PFPS). This article pointed out the prevalence of PFPS and misguided treatment on local factors. Before delving into treatment strategies, let’s discuss what factors can predispose an athlete to the injury.
General Etiology of PFPS
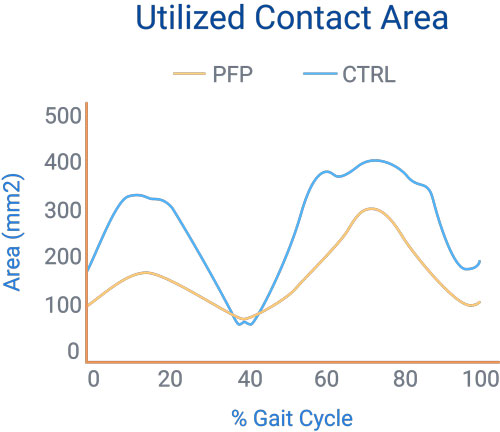
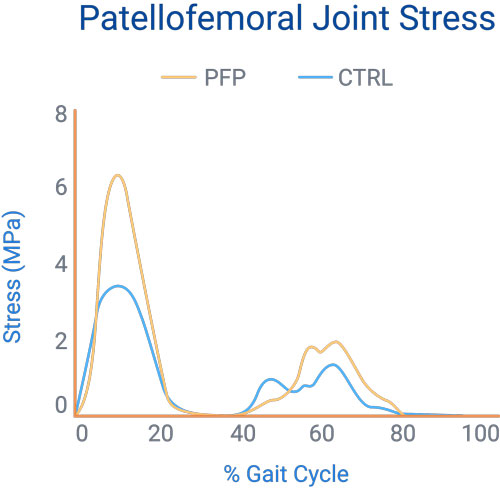
Biomechanically speaking, it comes down to a simple formula: Patellofemoral Joint (PFJ) Reaction Force / PFJ Contact Area = PFJ Stress
Contact Area
The contact area biomechanics have a strong impact on the amount of PFJ stress and are crucial for understanding its variability.
- As an individual goes into deeper ranges of knee flexion, their PFJ contact area increases.
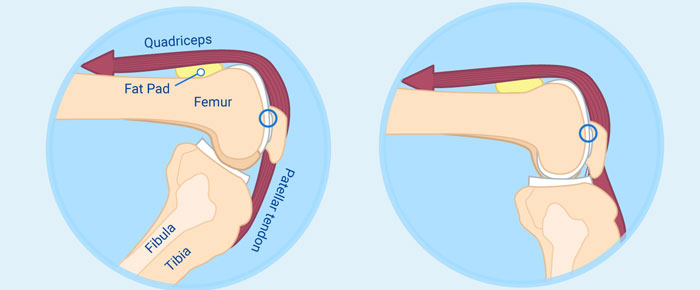
- During open kinetic chain knee flexion, the patella glides inferiorly to increase its contact with the femoral trochlea.
- During the closed kinetic chain, the femur rotates posteriorly causing increased contact with the patella.
Due to this variation in loading, the PFJ experiences some of the highest stresses in the body, especially during the lower ranges of knee flexion where the contact area is limited.
Altered Joint Loading
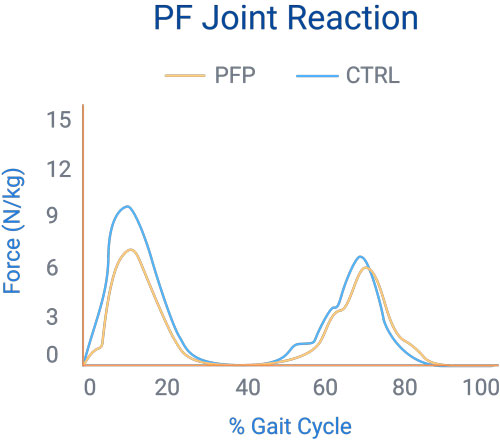
In 2002, Heino et al attempted to show that individuals with PFPS had altered joint loading that resulted in joint stress. They compared the PFJ reaction force, joint stress, and contact area during free and fast walking in subjects with PFPS and asymptomatic controls. On average, those with PFPS had the following characteristics:
- Lower joint reaction forces
These may be attributed to the patients’ unwillingness to forcefully load their affected limb, according to the researchers. - Higher joint stress and smaller contact area
These implicate that the improper loading may be causing the anterior knee pain in these patients.
PFPS Cascade
Thus, it follows that the general etiology of PFPS has a cascade pattern:
- Smaller PFJ contact area and higher reaction force → higher chondral stress
- Higher chondral stress → higher subchondral bone stress
- Higher subchondral bone stress → pain receptor stimulation
- Pain receptor stimulation → patellofemoral pain
The patellofemoral pain can be traced back to nociceptive afferent nerves located in the subchondral bone (Biedert et al).
Farrokhi et al (2011) gave further support to this theory that increased cartilage loading leads to its degeneration. They found that patella cartilage was significantly thinner in PFPS individuals compared to asymptomatic controls. Moreover, the PFPS individuals took more time to return to baseline cartilaginous thickness following an acute bout of exercise.
This is all well and good, but what causes this altered contact area?
1. Patella Alta (PA)
The abnormal loading may be caused by non-modifiable morphological abnormalities. According to Ward et al, patella alta increases the incidence of lateral displacement, lateral tilt, and decreased contact area. As to PFJ contact area, subjects with PA and those with normal patella vertical displacement showed statistically significant difference at all ranges tested (0°, 20°, 40°, and 60°of knee flexion).
This makes sense considering that the inferior pole of the patella is thought to make initial contact with the femoral trochlea at about 20° of knee flexion. If the patella is positioned more superiorly, initial contact will not occur until deeper ranges of knee flexion, thus decreasing overall PFJ contact area.
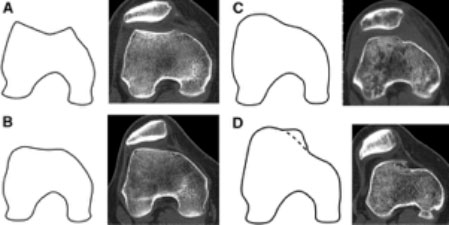
2. Trochlear Dysplasia
Another non-modifiable factor is trochlear dysplasia with corresponding lateral displacement and smaller contact area. This bony morphological defect results in flattening of the lateral facet of the intercondylar groove, which is typically the main local factor controlling excessive lateral patella translation. This can result in the following:
- Abnormal loading
- Recurrent (even possibly chronic) subluxation – dislocation
- Up to a 55% decrease in medial patellar stability
Unfortunately, there is very little that we can do to correct the above morphological abnormalities. We can, however, alter certain factors of abnormal patellar tracking conservatively, for example Q-angle and quadriceps dominance.
3. Static and Dynamic Q-Angles
The static Q-angle has been implicated in patellofemoral pathology for countless years, but how does it correlate to alignment during functional activity?
Recent findings favor using the dynamic measure in lieu of its static counterpart. Massada et al found that dynamic Q-angle was statistically significant in determining individuals who suffer from PFPS even when the static Q-angle was normal. There was little correlation between static Q-angle and the presence of PFPS in this study.
So what causes this altered dynamic Q-angle?
This angle is influenced proximally at the hip (excessive adduction and femoral IR) and distally at the ankle/foot (excessive pronation and tibial IR).
During weight-bearing, the femur moves about a fixed patella. Thus, excessive femoral IR localizes contact primarily to the lateral facet of the patella (Powers et al). In fact, just 10° of IR can substantially decrease the PFJ contract area and increase joint stress by 50%. The figure below demonstrates the lateral tilt of the patella during non-weight bearing (A) and the femoral IR altering the contact area during weight bearing (B).
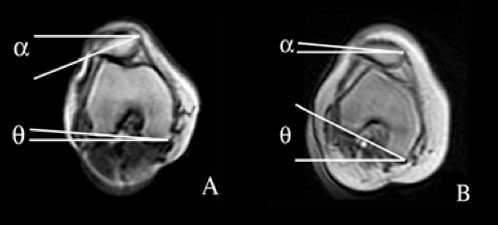
(A) lateral tilt of the patella during non-weight bearing; (B) femoral IR altering the contact area during weight-bearing.
Moreover, females with PFPS showed greater peak hip IR compared to the control group during running, drop jump, and step down (Souza et al). The hip abductors and extensors were weaker in the PFPS group, by 14% and 17% respectively.
Individuals with PFPS had increased hip adduction during running, jumping, and single-leg squats, according to Wilson et al, Noehren et al, and Nakagawa et al. This adduction increases valgus force about the knee joint, putting greater load on the lateral PFJ.
Distally, subtalar pronation can lead to IR of the tibia, which again increases the valgus at the PFJ.
4. Quadriceps Dominance (QD)
Last, but not least, QD has been shown to increase the incidence of PFPS due to the subsequent increased PFJ compression.
When landing from a jump, a QD individual will have their knees in front of their toes, excessive dorsiflexion, heels off of the ground, and limited hip flexion. This posture puts significant stress on the quadriceps and PFJ while taking stress off of the back and hip extensors.
Patients tend to adopt this compensation when their hip extensors are weaker than knee extensors. Such compensation will, in time, cause quadriceps overuse and increased knee loading, leading the patient down the above-mentioned cascade toward PFPS.
Pollard et al gave support to this theory when they found that greater use of hip extensors during a drop jump was associated with lower knee valgus angles and moments. Further, individuals who landed in a QD position had higher knee valgus and knee adduction moments, but lower energy absorption at the knee and hip. They were unable to properly dissipate the high ground reaction forces, ultimately putting unnecessary stress on the PFJ.
Beyond Biomechanics
Biomechanical factors make up only a piece of the puzzle. Each patient experiences pain differently based on their previous injury, fear avoidance behavior, and pain catastrophizing, among other factors.
However, with a better understanding of this pathology and its biomechanical factors, we can begin to enhance our conservative treatment strategies. These treatments should aim to decrease laterally directed PFJ forces (locally, proximally, and distally) and quadriceps dominance, while maximizing PFJ contact area.